Comparison of capability of data classification models to predict consistent results for depression analysis based on user-behaviour tracking and facial expression recognition during PHQ-9 assessment
Main Article Content
Abstract
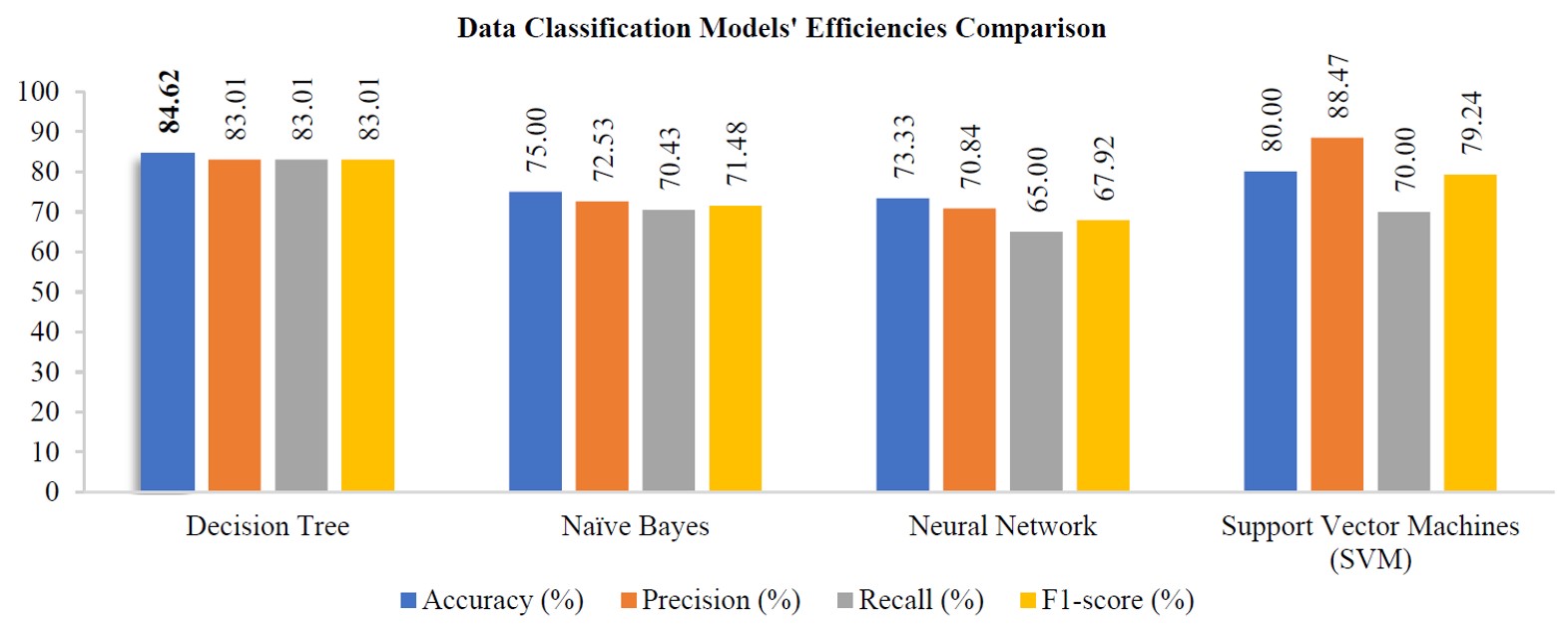
This research compares the capability of data classification models to predict consistent results for a subject’s depression potentiality, track the subject behaviour and recognise facial expressions during PHQ-9 assessments. This research is motivated by the necessity for depression screening and diagnosis, which traditionally relies on observations by experienced physicians or clinical psychologists of symptoms in conjunction with data from questionnaires. However, the field still requires a suitable technological approach that gives more accurate and consistent results. All data used in the present research were collected by combining technologies and compared by using classification models, the goal being to find the machine-learning model that most accurately predicts consistent results for the subjects’ PHQ-9 assessment, behaviours and emotions. The subjects were screened by clinical psychologists and divided into three groups: (i) subjects suffering from depression but not receiving treatment (undertreated subjects), (ii) subjects undergoing depression treatment (subjects undergoing treatment) and (iii) subjects without depression disorder (normal subjects). Related studies have compared the accuracy of classification models to one another. The four most frequently applied classification models in depression-related studies are (i) decision tree (ii) support vector machine, (iii) naïve Bayes and (iv) neural network. All models were analysed, designed and developed before being tested experimentally. The accuracy of the experimental results was tested by using the data analysis tool RapidMiner Studio. The results show that the decision tree model is not only the most accurate for predicting depression potentiality, tracking behaviour and recognising facial expressions during PHQ-9 assessments but also the most suitable.
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
References
Yang J, Zhang Z, Fu Z, Li B, Xiong P, Liu X. Cross-subject classification of depression by using multiparadigm EEG feature fusion. Comput Methods Programs Biomed. 2023;233:107360.
World Health Organization. Depression [Internet]. 2021 [cited 2021 Aug 5]. Available from: https://www.who.int/news-room/fact-sheets/detail/depression.
Zheng Y, Chen X, Li D, Liu Y, Tan X, Liang Y, et al. Treatment-naïve first episode depression classification based on high-order brain functional network. J Affect Disord. 2019;256:33-41.
Hossain S, Umer S, Rout RK, Tanveer M. Fine-grained image analysis for facial expression recognition using deep convolutional neural networks with bilinear pooling. Appl Soft Comput. 2023;134:109997.
Kanraweekultana N, Waijanya S, Promrit N, Korsanan A, Poolphol S. Depression analysis using behavior tracking and facial expression recognition during PHQ-9 assessment. ICIC Express Lett. 2023;17(3):303-14.
Faculty of Medicine Ramathibodi Hospital.Ramathibodi Essential Psychiatry. Bangkok: Mahidol University Press; 2015. (In Thai)
Li Y, Chu T, Liu Y, Zhang H, Dong F, Gai Q, et al. Classification of major depression disorder via using minimum spanning tree of individual high-order morphological brain network. J Affect Disord. 2023;323:10-20.
Liu YS, Song Y, Lee NA, Bennett DM, Button KS, Greenshaw A, et al. Depression screening using a non-verbal self-association task: a machine-learning based pilot study. J Affect Disord. 2023;310:87-95.
Souza Filho EM, Veiga Rey HC, Frajtag RM, Arrowsmith Cook DM, Dalbonio de Carvalho LN, Pinho Ribeiro AL, et al. Can machine learning be useful as a screening tool for depression in primary care?. J Psychiatr Res. 2021;132:1-6.
Dong W, He Y, Wang J, Shi C, Niu Q, Yu H, et al. Differential diagnosis of schizophrenia using decision tree analysis based on cognitive testing. Eur J Psychiatry. 2022;35(4):246-51.
Singh A, Kumar D. Detection of stress, anxiety and depression (SAD) in video surveillance using ResNet-101. Microprocess Microsyst. 2022;95:104681.
Price GD, Heinz MV, Zhao D, Nemesure M, Ruan F, Jacobson NC. An unsupervised machine learning approach using passive movement data to understand depression and schizophrenia. J Affect Disord. 2022;316:132-9.
Mahoto NA, Shaikh A, Sulaiman A, Reshan MSA, Rajab A, Rajab K. A machine learning based data modeling for medical diagnosis. Biomed Signal Process Control. 2023;81:104481.
Joshi ML, Kanoongo N. Depression detection using emotional artificial intelligence and machine learning: a closer review. Mater Today: Proc. 2022;58(1):217-26.
Kumar P, Garg S, Garg A. Assessment of anxiety, depression and stress using machine learning models. Procedia Comput Sci. 2020;171:1989-98.
Huang Y, Zhu C, Feng Y, Ji Y, Song J, Wang K, et al. Comparison of three machine learning models to predict suicidal ideation and depression among Chinese adolescents: a cross-sectional study. J Affect Disord. 2022;319:221-8.
Aleem S, Huda N, Amin R, Khalid S, Alshamrani SS, Alshehri A. Machine learning algorithms for depression: diagnosis, insights, and research directions. Electronics. 2022;11(7):1111.
Faculty of Medicine Ramathibodi Hospital. PHQ-9 Depression Assessment [Internet]. 2022 [cited 2021 Aug 5]. Available from: https://www.rama.mahidol.ac.th/th/depression_risk. (In Thai)
Uddin MZ, Dysthe KK, Følstad A, Brandtzaeg PB. Deep learning for prediction of depressive symptoms in a large textual dataset. Neural Comput Appl. 2022;34:721-44.
Sun Y, Fu Z, Bo Q, Mao Z, Ma X, Wang C, et al. The reliability and validity of PHQ-9 in patients with major depressive disorder in psychiatric hospital. BMC Psychiatry. 2020;20:474.
Dede B, Delk L, White BA. Relationships between facial emotion recognition, internalizing symptoms, and social problems in young children. Pers Individ Differ. 2021;171:110448.
Panichkriangkrai C, Silapasuphakornwong P, Saenphon T. Emotion recognition of students during e-learning through online conference meeting. Sci Eng Health Stud. 2021;15:1-10.
Scoppetta O, Cassiani-Miranda CA, Arocha-Díaz KN, Cabanzo-Arenas DF, Campo-Arias A. Validity of the patient health questionnaire-2 for the detection of depression in primary care in Colombia. J Affect Disord. 2021;278:576-82.
Faculty of Medicine Ramathibodi Hospital. Depression in detail [Internet]. 2022 [cited 2021 Aug 5]. Available from: https://med.mahidol.ac.th/ramamental/generalknowledge/ general/09042014-1017. (In Thai)
Costantini L, Pasquarella C, Odone A, Colucci ME, Costanza A, Serafini G, et al. Screening for depression in primary care with Patient Health Questionnaire-9 (PHQ-9): a systematic review. J Affect Disord. 2021;279:473-83.
Visser LNC, et al. Methodological choices in experimental research on medical communication using vignettes: the impact of gender congruence and vignette modality. Patient Educ Couns. 2022;105(6):1634-41.