Assessing the Relationship and Effect of Air Pollution [PM 2.5] on Child Respiratory Illness and Child Mortality in the Philippines
Main Article Content
Abstract
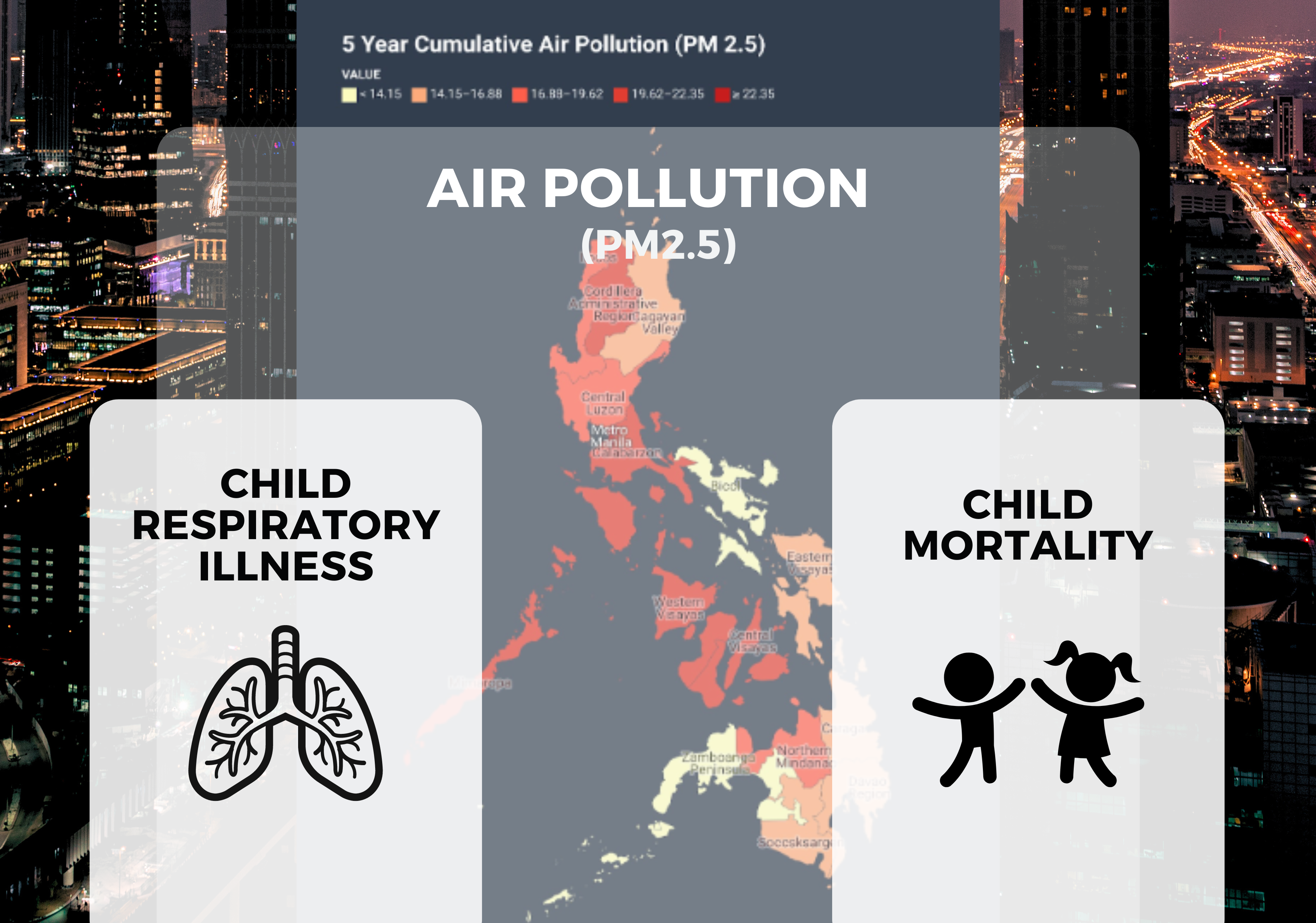
Air pollution is the presence of harmful substances in the air, which can seriously impact human health and the environment. Among the air pollutants, fine particulate matter (PM) 2.5, being a microscopic particle, poses serious health risks since it can enter the blood circulation and go deep into the lungs. PM 2.5 has been linked to several health problems, such as early mortality, problems with children's development, and unfavorable birth outcomes. In this regard, the study aims to investigate the relationship and effect of PM 2.5 on child respi-ratory illness and child mortality in the Philippines. Data on child respiratory illness and mortality were sourced from the 2022 Philippine National Demo-graphic and Health Survey by the Philippine Statistics Authority. PM 2.5 data was obtained from the official website of the Department of Environment and Natural Resources' Environmental Management Bureau (DENR-EMB). Choropleth map, correlation plot, and regression analysis were used to analyze the data. Results reveal that regions with the greatest number of highly urbanized cities and greater industrial and economic activities have higher levels of PM 2.5. The relationship is positive and significant between PM 2.5 and child respiratory illnesses. (Acute respiratory illness, r=0.87; Asthma, r=0.90) and child mortality (neonatal mortality, r=0.72; post neonatal mortality, r=0.71; under five mortality, r=0.61). As PM 2.5 levels increase, the rates of child respiratory illnesses and child mortality are also expected to increase. Mitigating elevated PM 2.5 levels in urban settings necessitates a collaborative approach involving government agencies, industries, communities, and individuals. By integrating regulatory measures, embracing technological innovations, fostering public awareness, and promoting community engagement, it is feasible to alleviate the adverse effects of air pollution on children's health and the general well-being of the public.
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Published articles are under the copyright of the Applied Environmental Research effective when the article is accepted for publication thus granting Applied Environmental Research all rights for the work so that both parties may be protected from the consequences of unauthorized use. Partially or totally publication of an article elsewhere is possible only after the consent from the editors.
References
Analitis A, Katsouyanni K, Dimakopoulou K, et al. Short-term effects of ambient particles on cardiovascular and respiratory mortality. Epidemiology 2006;17:230-3.
Anwar, A., Ullah, I., Younis, M., & Flahault, A. (2021). Impact of air pollution (PM2. 5) on child mortality: Evidence from sixteen Asian countries. International Journal of Environmental Research and Public Health, 18(12), 6375.
Brunekreef B, Holgate ST. Air pollution and health. Lancet 2002;360:1233-42.
Dominici F, Peng RD, Bell ML, et al., Fine particulate air pollution and hospital admission for cardiovascular and respiratory diseases. JAMA 2006;295:1127-34.
Eze IC, Schaffner E, Fischer E, Schikowski T, Adam M, Imboden M, et al.. Long-term air pollution exposure and diabetes in a population-based Swiss cohort. Environ Int. (2014) 70:95–105. 10.1016/j.envint.2014.05.014
Environmental Management Bureau. (2023). PM 2.5 Annual Historical Data. https://emb.gov.ph/air-quality-data/
Ghorani-Azam, A., Riahi-Zanjani, B., & Balali-Mood, M. (2016). Effects of air pollution on human health and practical measures for prevention in Iran. Journal of research in medical sciences: the official journal of Isfahan University of Medical Sciences, 21.
Ho, Y. N., Cheng, F. J., Tsai, M. T., Tsai, C. M., Chuang, P. C., & Cheng, C. Y. (2021). Fine particulate matter constituents associated with emergency room visits for pediatric asthma: A time-stratified case–crossover study in an urban area. BMC Public Health, 21, 1-8.
Huynh M, Woodruff TJ, Parker JD, et al. Relationships between air pollution and preterm birth in California. Paediatr Perinat Epidemiol 2006;20:454-61
Kurt, O. K., Zhang, J., & Pinkerton, K. E. (2016). Pulmonary health effects of air pollution. Current opinion in pulmonary medicine, 22(2), 138.
Malley, C. S., Kuylenstierna, J. C., Vallack, H. W., Henze, D. K., Blencowe, H., & Ashmore, M. R. (2017). Preterm birth associated with maternal fine particulate matter exposure: a global, regional and national assessment. Environment International, 101, 173-182.
Manisalidis, I., Stavropoulou, E., Stavropoulos, A., & Bezirtzoglou, E. (2020). Environmental and health impacts of air pollution: a review. Frontiers in public health, 8, 14.
Morales-Ancajima, V. C., Tapia, V., Vu, B. N., Liu, Y., Alarcón-Yaquetto, D. E., & Gonzales, G. F. (2019). Increased outdoor PM2.5 concentration is associated with moderate/severe anemia in children aged 6–59 months in Lima, Peru. Journal of Environmental and Public Health, 2019.
National Demographic and Health Survey (2022). Philippine Statistics Authority. https://dhsprogram.com/pubs/pdf/FR381/FR381.pdf
Odo, D. B., Yang, I. A., Dey, S., Hammer, M. S., van Donkelaar, A., Martin, R. V., ... & Knibbs, L. D. (2022). Ambient air pollution and acute respiratory infection in children aged under 5 years living in 35 developing countries. Environment International, 159, 107019.
Shiferaw, A. B., Kumie, A., & Tefera, W. (2023). Fine particulate matter air pollution and the mortality of children under five: a multilevel analysis of the Ethiopian Demographic and Health Survey of 2016. Frontiers in Public Health, 11, 1090405.
Spears, D., Dey, S., Chowdhury, S., Scovronick, N., Vyas, S., & Apte, J. (2019). The association of early-life exposure to ambient PM2. 5 and later-childhood height-for-age in India: an observational study. Environmental Health, 18(1), 1-10.
Tainio, M., Andersen, Z. J., Nieuwenhuijsen, M. J., Hu, L., De Nazelle, A., An, R., ... & de Sá, T. H. (2021). Air pollution, physical activity and health: A mapping review of the evidence. Environment International, 147, 105954.
Wen, X. J., Balluz, L., & Mokdad, A. (2009). Association between media alerts of air quality index and change of outdoor activity among adult asthma in six states, BRFSS, 2005. Journal of Community Health, 34(1), 40-46.
Wilson WE, Suh HH. Fine particles and coarse particles: concentration relationships relevant to epidemiologic studies. J Air Waste Manag Assoc. (1997) 47:1238–49. 10.1080/10473289.1997.10464074
Woodruff, T. J., Parker, J. D., & Schoendorf, K. C. (2006). Fine particulate matter (PM2. 5) air pollution and selected causes of postneonatal infant mortality in California. Environmental health perspectives, 114(5), 786-790.
Xie, G., Sun, L., Yang, W., Wang, R., Shang, L., Yang, L., ... & Chung, M. C. (2021). Maternal exposure to PM2. 5 was linked to elevated risk of stillbirth. Chemosphere, 283, 131169.
Xing, Y. F., Xu, Y. H., Shi, M. H., & Lian, Y. X. (2016). The impact of PM2. 5 on the human respiratory system. Journal of thoracic disease, 8(1), E69.
Yang, L., Li, C., & Tang, X. (2020). The impact of PM2. 5 on the host defense of respiratory system. Frontiers in cell and developmental biology, 8, 91.
Zanobetti A, Franklin M, Koutrakis P, et al. Fine particulate air pollution and its components in association with cause-specific emergency admissions. Environ Health 2009;8:58.